Prevention and Clinical Management of Rape Survivor
What is Rape?
Rape is defined as “unlawful sexual intercourse or any other sexual penetration of the vagina, anus, or mouth of another person, with or without force, by a sex organ, other body part, or foreign object, without the consent of the victim”.

Prevention Tips of Rape: :
- Don’t put drugs in women’s drinks.
- When you see a woman walking by herself, leave her alone.
- If you pull over to help a woman whose car has broken down, remember not to rape her.
- If you are in an elevator and a woman gets in, don’t rape her.
- When you encounter a woman who is asleep, the safest course of action is to not rape her
- Never creep into a woman’s home through an unlocked door or window, or spring out at her from between parked cars, or rape her.
- Remember, people go to the laundry room to do their laundry. Do not attempt to molest someone who is alone in a laundry room.
- Use the Buddy System. If it is inconvenient tor you to stop yourself from raping women, ask a trusted friend to accompany you at all times.
- Carry a rape whistle. If you find that you are about to rape someone, blow the whistle until someone comes to stop you.
- Don’t forget: Honesty is the best policy. When asking a woman out on a date, don’t pretend that you are interested in her as a person: tell her straight up that you expect to be raping her later. If you don’t communicate your intentions, the woman may take it as a sign that you do not plan to rape her.
Clinical Management of Rape Survivor:
Step 1: Prepare the survivor for examination
- Take a private consultation room.
- Offer comfort and understanding.
- Explain procedures and get informed consent.
- Seek approval before each and every procedure performed.
Step 2: Take medical history
- Review paperwork brought by the survivor to not repeat any point already documented.
- Avoid questions that suggest blame or judgment.
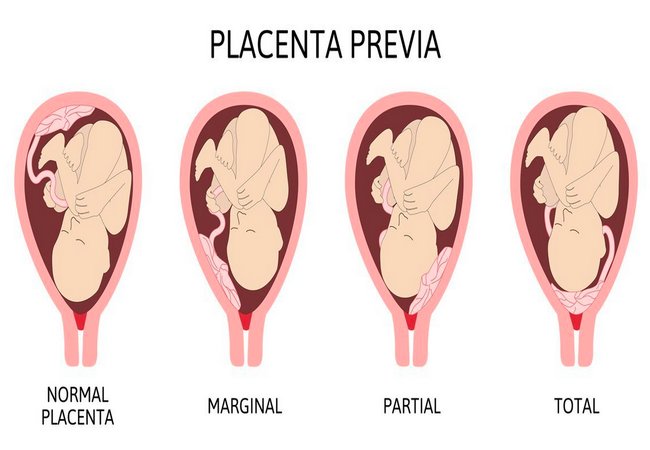
- Explore possibility of pre-existing pregnancy.
Step 3: Collect forensic evidence (up to 72 hours)
- Only if survivor agrees.
- Only if evidences can be processed.
Step 4: Conduct physical examination
- Examine survivor gently and systematically.
- Note size, colour and locations of injuries.
- Look for signs of pre-existing pregnancy.
Step 5: Provide treatment
- Counsel and get consent on treatment.
- Give PEP (up to 72 hours), counsel on HIV testing.
- Give EC or insert copper-IUD (up to 120 hours) to women with no pre-existing pregnancy.
- Give STIs prophylaxis.
- Vaccinate for tetanus and hepatitis B.
- Treat wounds step.
Step 6: Conduct physical examination
- Examine survivor gently and systematically (depending on the time line this will be more or less appropriate, see full protocol for details).
- Note size, colour and locations of injuries.
- Look for signs of pre-existing pregnancy.
Step 7: Provide treatment
- Counsel and get consent on treatment.
- In case of pregnancy, help to determine if it is from rape (it might not be possible). Counsel on the way forward.
- Give STIs prophylaxis (up to 2 weeks) or provide syndromic treatment as relevant.
- Test for HIV if at least 3 months after rape.
- Give tetanus and hepatitis B prophylaxis as appropriate.
- Treat unhealed wounds.
Step 8: Provide psychological first aid and counseling
- Identify survivor protective factors, risk factors and copying mechanisms.
- Look for psychological distress signs and symptoms; Listen actively; Link and support referral to services and assistance.
- Give clear and simple instructions for medications, wounds care, and follow-up.
Step 9: Make a medical certificate
- Provide a certificate to the survivor and keep a copy.
Step 10: Provide follow-up care
- Follow-up according to initial findings, treatments prescribed, pregnancy, injuries.
Documentation:
- Document the survivor’s physical exam, history and treatment using standardized forms.
- Keep the documentation and evidence in a secure and confidential place.
- Do not share any nominative information without the survivor’s consent.
- Record case in the health information system in an anonymous manner.